Why You Shouldn’t Ignore the Mind-Body Connection
Stacey J. Drubner, JD, LICSW, MPH

EAP Ask the Expert: Darshan Mehta, MD, MPH, Medical Director, Benson-Henry Institute for Mind Body Medicine, Director, Office for Well-Being, Center for Faculty Development at Massachusetts General Hospital, & Education and Medical Director, Osher Center for Integrative Medicine at Brigham & Women’s Hospital
According to the American Psychological Association’s 2023 Stress in America Survey:
- The majority of respondents rate their stress at 5/10, with about a quarter of respondents rating their stress somewhere between 8/10 – 10/10
- 62% keep their stress to themselves as they don’t want to burden others
The reason that these statistics matter is that prolonged, unchecked stress has a significant impact on the body and overall health. This cause-and-effect relationship is part of the mind-body connection (MBC).
Some may brush over the concept of the MBC because they think they must be a yoga or meditation expert to experience an impact. The truth is that anyone who struggles with stress can improve their health status by addressing unproductive patterns and maximizing the MBC.

In this month’s feature, we once again tap into the expertise of Dr. Darshan Mehta to explore the mind-body connection and why it is so crucial to health and functioning. We will cover some concrete examples of how stress can impact the body and how best to protect our well-being and respond to stress.
What is the Mind-Body Connection & Why Does it Matter?
The National Institutes for Health (NIH) describes the MBC via the following:
- “Interactions among the brain, mind, body, and behavior, and the powerful ways in which emotional, mental, social, spiritual, and behavioral factors can directly affect health.”
– In other words, how we think, act, and care for our bodies feeds off each other. A healthy mind results in a healthy body and vice versa. In a recent feature, we highlighted how physical health affects brain health. For example, we learned how controlling cholesterol, blood pressure, and diabetes can potentially prevent strokes and dementia.
- The second part of the definition “regards as fundamental, an approach that respects and enhances each person’s capacity for self-knowledge and self-care, and it emphasizes techniques that are grounded in this approach.”
– Dr. Mehta underscores that this gives us the power to impact our health and well-being rather than depending on someone else to control it. We can be in the driver’s seat.
How Stress fits in with the Mind-Body Connection
Stress is an important component in the MBC because, left unchecked, it can have effects on several levels:
- The brain
- The genes – such as inflammatory markers
- Downstream via localized health consequences
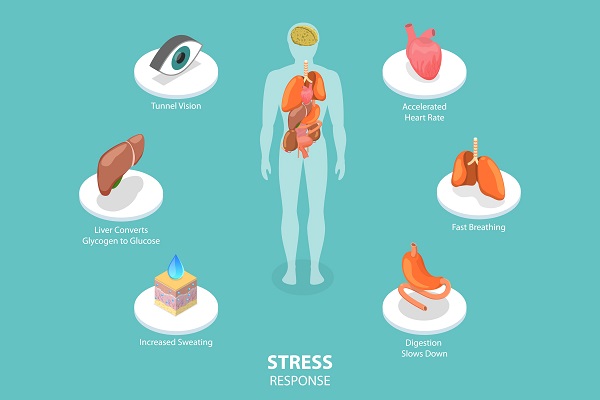
It’s important to differentiate between necessary or “beneficial stress” and an unhealthy stress response. There are circumstances when you need to activate this system for survival, such as encountering a bear while on a hike. This is an excellent time to trigger your internal survival mechanism (flight or fight). Darshan explains that problems arise when the stress response is activated too often, sometimes without an actual stressor. This can release high adrenaline and cortisone levels and compromise your ability to adapt and access the appropriate response when needed. This imbalance eventually causes the MBC to be out of sync and impacts health.
Research Supporting the Importance of the Mind-Body Connection
There is a lot of buzz about the MBC due in part to recent research. Our understanding of the MBC and its scientific support has evolved significantly since philosopher Descartes first considered the idea in the 17th Century. Contributions by others, such as MGH’s Dr. Herbert Benson, gave the MBC credibility in healthcare. Today, the knowledge base continues to grow, and the research drills down even more on the systems and processes impacting the MBC. There are too many studies to mention, but we list some below, including research from Mass General Brigham:

- MGH – The Risk Between Stress & Cardiovascular Disease
- AHA – Depression, Anxiety, and Stress Linked to Poor Heart Health
- BWH – Emotional Wellbeing May be Directly Linked to Women’s Gut Health
- Washington University School of Medicine – The Mind-body Connection is Built into the Brain
- BIDMC – Mindfulness Impacts on Back Pain
- MGH – 5 Health Benefits of Meditation
Warning Signs that the Mind-Body Connection is out of Sync
Darshan suggests looking for persistent impacts in any of the following domains:
- Thoughts
–An over-focus on negative ideas, such as the belief that you are not good enough or don’t belong
- Emotions
–Sadness, anger, irritability, worry, fear
- Behavior
–Unhealthy eating or use of substances
- Physical symptoms
–Pain, fatigue, sleep issues, headaches, stomach problems, weakened immune system, cardiac issues
- Relational
–Isolating from your support network or finding fault with people more easily
Steps to Take to Fortify the Mind-body Connection and Minimize Stress

Below, we list areas that are most relevant to a healthy MBC. Most of us have a sense of what we are supposed to do to maximize health and well-being. The challenge is in how to go about it. Trying to address everything at once can be daunting. Consider evaluating your priorities based on your capabilities, health concerns, and schedule. Don’t try to tackle too many things at once. Our feature on healthy habits has some tips for approaching this process.
- Healthy lifestyle
- Mindfulness and stress reduction practice
–Yoga
- Social connection
- Daily gratitude/appreciation
- Reduction of unhealthy behaviors, such as using substances to cope
How Providers can Help Patients with the Mind-body Connection

One of the most essential steps clinicians can take is acknowledging and normalizing the MBC. Make it part of your routine screening and communicate that how patients handle stress will affect critical indicators of health such as blood pressure, gut functioning, pain, and mental health (anxiety and depression). This is no longer an issue that should be addressed only in a holistic space. Whether you work in primary care or a specialty practice, chances are you will engage with many people who have untreated stress and are reporting medical side effects resulting from this stress. Darshan highlights the thoughts of long-time physician Dr. John Stoeckle, who found that 60-90% of ambulatory visits are related to stress.
- Educate yourself and stay updated on the MBC knowledge base and root causes of challenges
- Talk about the MBC with patients and how it can improve or jeopardize their well-being
- Use a non-judgmental approach to encourage patients to be open to discussing tough topics such as weight management or substance use
- Encourage patients to seek the help of a professional when they:
-Keep doing the same thing without seeing any improvement
-Feel overwhelmed
-Are curious and want to know more
Resources
- MGB Well-being Offerings
- EAP Wellness Resources
- EAP Healthy Lifestyle Resources
- Benson Henry Institute for Mind-Body Medicine – MGH
- The Osher Center for Integrative Medicine – BWH
- Other Recent EAP Well-being Features:
–Steps You Can to Protect Your Brain Health Today and in the Future
–Find Healthy Habits that Work for You
–If you want to Improve your Health, Improve your Sleep
–The Drawbacks of Using Alcohol to Cope
–Why is Everyone Talking about Mindfulness
–Getting Back on Track with Healthy Eating
–Is Marijuana as Safe as You Think it is?
Help from the EAP
The EAP offers free and confidential services for employees and immediate household family members. EAP records are separate from medical and HR records. Contact the EAP at 866-724-4327 or request an appointment via our online form for confidential assistance. In-person appointments are available at the following locations. Phone or Video (Zoom) appointments are available from all locations.