Understanding Early Onset Cancer in Younger Adults
Stacey J. Drubner, JD, LICSW, MPH
EAP Ask the Expert: Lecia Sequist, MD, MPH – Oncologist and Program Director, Cancer Early Detection and Diagnostics Clinic, Massachusetts General Hospital*
Historically the idea of certain kinds of cancer (breast, colon, lung) affecting someone in their 30’s or 40’s seemed fairly unusual. Recent attention on early-onset cancers (generally affecting those aged 18-49) has been prompted by stories of well-known individuals, such as Kate Middleton or Chadwick Boseman having cancer. Unfortunately, these cases are not outliers.
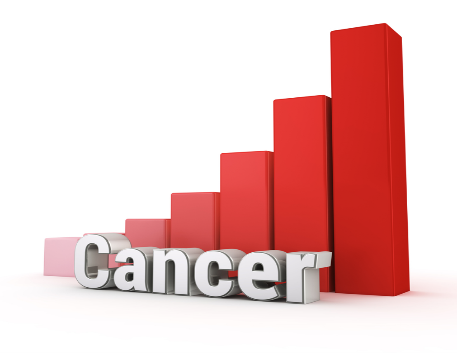
According to JAMA, analysis from National Cancer Institute data from 2010-2019 in the US, shows an increase (+.74%) in overall early-onset cancer diagnoses. The same study indicated that women (+4.35%) and people in their 30’s experienced the biggest increases.
The most common early-onset cancers (some of which are rising 1-2% annually) include:
- Gastrointestinal and colorectal cancers, which have the most significant and concerning rate increases
- Breast cancers, with the biggest jump in the number of cases
- Urinary cancers
- Reproductive system cancers, such as ovarian or uterine cancers
The American Cancer Society (ACS) reported that breast cancer and colorectal cancer account for the most common early-onset cancer deaths in women and men respectively.
To find out what might be behind these early-onset cancer trends and learn about some keys to prevention and successful treatment, we turned to Dr. Lecia Sequist, oncologist from MGH.
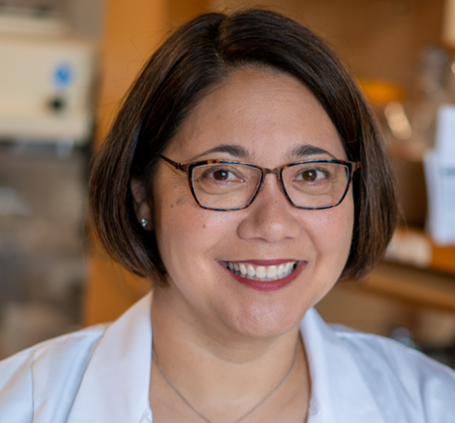
Dr. Sequist explains that overall, cancer still affects older individuals (over 50) much more because the safety mechanisms that naturally help us prevent cancer become less effective as we age. Researchers and clinicians are still in the initial stages of understanding the steady percentage increase in cancers in people under 50. One consideration to keep in mind is that cancer is not one disease, but several conditions that affect many different organs and systems.
Are the Presentations of Cancer in Younger People Different?
Some clinics are reporting more aggressive forms of cancer in some early-onset cases. On the one hand, this might be due to the origins of the disease, but in some cases, it’s likely a function of later diagnosis. Cancers are typically found in one of two ways that are not necessarily targeted towards younger patients:
- The patient has symptoms and consults with a medical provider and tests are performed
In this scenario, a younger patient may not engage with a doctor because they may be busy or under the impression that they wouldn’t have a serious medical condition. The provider may not view a young patient as being high-risk for cancer and might take a “wait and see” approach or provide a non-invasive treatment (antibiotics) before looking for cancer.
- Screening test when people have no symptoms
Many younger patients do not meet routine screening requirements, which are based on age, so there is no opportunity to catch asymptomatic cases before the cancer becomes more advanced.
What do we know about Risk Factors for Early Onset Cancers?
Historically, the conventional wisdom around cancer risk was somewhat simplistic. For example, those who smoked/used tobacco products were at high-risk for lung cancer, and those who never smoked were considered to be low risk. We now know that many lung cancer patients lack a history of tobacco use. Similarly, younger age is no longer considered to be as protective when it comes to certain conditions, such as colon cancer. Today, our understanding of risk is more nuanced and fluid.
Dr. Sequist indicates that risk factors fall into two categories- those (family history, other medical conditions, environmental factors) that we do not have control over and those (lifestyle choices) that we have some control over.
Family history
An understanding of genetic predispositions for cancer allows you to:
- Have advance awareness of potential risk
- Take preventative steps, such as screening before the recommended age for the general population
- Catch and treat cancers in early stages
Dr. Sequist cautions that while family history is important it’s certainly not the only risk factor for cancer. Focusing on family history alone may provide a false sense of security and a tendency to disregard other risk factors like those referenced below. For example, public health messaging about the hereditary connection for breast cancer was so effective that some are not aware that only 5-10% of breast cancer is attributed to family history. The result is that some women may not be as diligent with mammograms in the absence of a family history.
Considerations about genetic testing

Genetic testing, which looks for changes (mutations) in your DNA, can be useful to identify disease risk and allow for earlier screening, identification, and intervention. Dr. Sequist indicates that genetic testing is becoming more commonly recommended, especially when thinking about cancer risk. It’s most relevant to people with a family history but cannot speak to environmental causes. Breast and colon cancers are most recognized as potentially being hereditary but genetic pre-dispositions are also being identified in other kinds of cancer.
Some possible downsides:
- Although testing is becoming more accessible and affordable, it’s not always covered by insurance
- Depending on the type of policy, results of testing could potentially impact life insurance coverage
Inevitably decisions about genetic testing will depend on what you and your provider determine is best for you.
Here are some resources in the MGB system:
- BWH – Genetics & Genomic Medicine Service
- MGH – Cancer Early Detection and Diagnostics Clinic
- MGH – Genetics and Genomics
Other medical conditions and treatments
Some aspects of your medical history can represent a potential risk for cancer. These can include:
- A previous cancer diagnosis
- Chronic inflammation, related to diseases like rheumatoid arthritis or inflammatory bowel diseases
- Medications that are immune-suppressive
Environmental factors
It’s not always easy to make the direct connection between environmental factors and cancer risk, but research in this area is becoming more robust. Dr. Sequist stresses that we are developing a greater appreciation of how poverty, stress, neighborhoods that you live in, air or water pollution and exposure to certain chemicals can pre-dispose us for disease.
Lifestyle choices

There are definitely steps everyone can take to minimize the chances of getting cancer, particularly around lifestyle habits that can lead to improved health status. This is relevant to many conditions, including cancer, heart disease, diabetes, mental health and cognitive functioning. Some of the most relevant to cancer prevention include:
- Avoiding smoking and vaping of tobacco or marijuana
- Limiting alcohol use
- Maintaining a healthy diet and avoiding obesity
- Engaging in regular exercise
- Avoiding sun exposure
In order to limit stigma and increase the likelihood of seeking help, it’s vital that the medical system and society at large remain supportive and non-judgmental of those who use tobacco or alcohol, or are obese. The causes of these conditions are complex, and do not always reflect simple personal choices. Before and after a cancer diagnosis, dialogue should be open and trigger no shame.
Steps you can Take to Prevent or Catch Cancer Early
Recognize and act on warning signs
Since younger people may not have health problems on their radar, it’s helpful to understand when to contact a medical provider for an evaluation. Any persistent symptom that is not resolving in two months or more warrants a consultation. This could include:
- Pain
- A cough that’s out of the ordinary and not due to a chronic condition such as asthma
- Changes in bowel habits
- Weight loss when not trying
Don’t be shy about asking for a professional opinion or a work-up for symptoms that are concerning. You are the #1 expert about you and should be an advocate for your own health and well-being.
Maintain a healthy lifestyle
As discussed above, a healthy lifestyle is one of the ways you can take an active role in your own well-being. Consider limiting use of alcohol and tobacco and maintaining a healthy weight.
Here are some resources from the EAP:
- EAP Healthy Lifestyle Section
- Finding Healthy Habits that Work for You
- Alcohol Use Resources
- Smoking Cessation Supports
- Getting Back on Track with Healthy Eating
- Guidance for Exercising
Learn how your genetic predispositions and previous health history affect cancer risk
- Take note of your family and personal history
- Consider genetic testing
Be vigilant about screening
- Keep informed of routine screening recommendations and changes in guidance
- Is there something in your family or medical background that warrants earlier screening?
- Does your current clinical presentation indicate that screening makes sense even if you are below the standard age cut-off?
Here are some screening guidelines. Please be aware that different professional organizations or societies might have varied recommendations. We list initial routine screening age (when there is a recommend one) based on normal risk.
- American Cancer Society – across all cancers
- Breast cancer
–Begin at age 40
- Cervical cancer
– Begin at age 21
- Colorectal cancer
– Begin at age 45
Don’t let fear lead to avoidance
There is a good chance that your symptoms are not a sign of a serious illness and it’s only natural to want to avoid negative news. However, if something is wrong, fast-tracking diagnosis and intervention will likely lead to more treatment options and better outcomes.
Dr. Sequist indicates that cancer treatments are going through a revolution. There are more targeted and less invasive interventions being studied and approved all the time. Your provider can tailor your treatment to your life stage and needs. For example, if fertility is a concern, that can be figured into your care plan.
Help from the EAP
The EAP offers free and confidential services for employees and immediate household family members. EAP records are separate from medical and HR records. Contact the EAP at 866-724-4327 or request an appointment via our online form for confidential assistance. In-person appointments are available at the following locations. Phone or Video (Zoom) appointments are available from all locations
* The content in this news feature is intended for informational purposes and is not meant to provide any specific clinical guidance. Every health care situation is unique and best addressed in consultation with your provider.