Understanding Treatment Options for Menopause
Stacey J. Drubner, JD, LICSW, MPH
EAP Ask the Expert, Tara K. Iyer, MD, Medical Director – Menopause and Midlife Clinic, Division of Women’s Health, Brigham and Women’s Hospital
For years, there has been significant attention on age-related hormone changes and impacts (sexual dysfunction) in men. In comparison, there has been relatively less focus on Perimenopause (transition to Menopause) and Menopause. These stages are triggered by reproductive system and hormone changes (production of progesterone and estrogen) in women. Societal norms around keeping discussions in the shadows, and a medical system that did not allot adequate clinical, training or research resources to these issues has led to:
- Less clarity on appropriate treatments & a lack of understanding about how menopause affects aging and related health complications
- Barriers to support
- Stigma
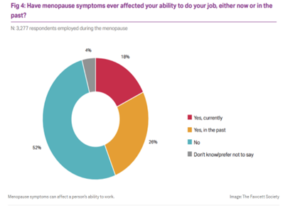
The cumulative impact is that many women have suffered unnecessarily. In addition to physical side effects (discussed in detail below), there are other impacts on quality of life, relationships, activities and even job satisfaction. A Mayo Clinic study reported an estimated $1.8 billion in lost work time per year in the US.
While there has been a recent shift signaling an increase in attention on Menopause, there is still conflicting and evolving guidance about treatment.

Dr. Tara Iyer, from Brigham & Women’s Hospital, has been working to put Menopause in the forefront of clinical care and medical education. In this month’s feature, she helps to synthesize options to address the short and long-term effects of Menopause. *
How is Menopause Diagnosed or Defined

Typically, providers make a clinical diagnosis via patient history, rather than lab tests to determine that someone is in natural menopause. Dr. Iyer indicates that a diagnosis of Menopause can be made if there is a 12-month span without a period. Sometimes lab work is needed for women who have had a hysterectomy or other procedures such as ovary removal. Determining that a patient is in Perimenopause is a little vaguer and involves a review of changes in cycle and accompanying symptoms.
Symptoms & Side-effects
There are multiple symptoms that may be associated with Perimenopause and Menopause. Some (such as hot flashes) are primarily hormone related. Many others, such as brain fog, may result from other factors too. It is likely that symptoms co-occur and feed off each other. For example, sleep and diet patterns are inter-connected and both can impact mood, cognition, weight and hot flashes. Some of the most common symptoms are listed below.

-Dr. Iyer points out that the risk of sleep disorders (sleep apnea) increases during and after the menopause transition. Interrupted sleep can result primarily from hormone changes or can be due to other secondary symptoms such as urinary issues or anxiety.
- Fatigue, low energy & joint pain
- Mood & mental health impacts
- Brain fog
-Many women report cognitive challenges, such as poor memory or lack of clear thinking. Research has not identified a definitive link, but one hypothesis is that lack of sleep leads to cognitive effects. Typically, these symptoms are temporary. There is not a proven connection around longer-term impacts- dementia – for those who reach Menopause at the expected age. However, those who go through Menopause early (before 40), may be at more risk for developing dementia.

-An increase in weight may be attributable to metabolism changes and other impacts, such as sleep disturbance, which can coincide with unproductive eating patterns. While there is no clear agreement on how much Menopause has a role in weight gain, there is greater consensus about changes in body composition and where and how weight is stored. Typically, weight is redistributed to the mid-section and the ratio of body fat to lean muscle shifts to an increase in fat.
- Incontinence
- Intimacy issues related to:
-Vaginal dryness, pelvic pain
-Sex drive
-Sleep deprivation
-Changes in mood
-Dr. Iyer refers to the impact of loss of estrogen on organ systems, including the heart and cardio-metabolic processes. With aging, women may experience spikes in cholesterol and blood pressure, resulting in blood flow issues, and potential cardiac disease. For the first half of life, men seem to be at higher risk for heart disease, but women catch up after mid-life hormone changes
– Menopause significantly speeds up the bone loss process and increases the risk of Osteoporosis (a progressive condition in which bones become structurally weak and are more likely to fracture or break). Dr. Iyer explains that the greatest decrease in bone mass occurs in the first 5 years of Menopause
Minimizing Symptoms & Long-term Health Issues
Below we discuss some common options to address Menopause symptoms and potential future health effects, but first a few words about treating Perimenopause. Dr. Iyer points out that Perimenopause symptoms can be more complicated to treat. While Menopause typically comes with consistently low hormone levels, Perimenopause has fluctuation in hormones, especially estrogen. This results in breast tenderness, mood swings, migraines and heavier bleeding. Ideal intervention involves meeting the patient where they are in response to changing symptoms, via:
- Birth control pills
- IUDs
- Hormone therapy (HT), which involves replenishing hormones that are reduced with age
Menopausal Hormone Therapy

The decision (and timing, type) to use HT will vary based on each women’s medical history, symptoms and age. Generally, the best benefit to risk ratio is realized when hormone therapy is started within 10 years of the beginning of menopause and before age 60.
Commonly, providers will prescribe a hormone package which includes estrogen and progestogen. Those who have had a hysterectomy and have no uterus typically only need estrogen therapy. Hormones may be either biosimilar (plant-based) or a synthetic (chemical formulation). Dr. Iyer cautions that compounded hormones are not FDA approved nor are they recommended by any of the relevant medical societies.
There are different delivery mechanisms and formulations including:
- Local (vaginal administration)
-Usually not systemic, as they are not absorbed into the blood stream - Patches & rings
- Pills
- Gels & creams
Below, we discuss the risks and benefits of HT with the caveat that research for the newer biosimilar hormones is evolving and some of the traditional red flags were related to older formulations.
Benefits
In the short-term there may be an improved quality of life, due to addressing symptoms:
- Hot flashes, night sweats
- Mood swings
- Intimacy issues
There may also be positive impacts on secondary side effects such as
- Sleep
- Weight impacts
In the Longer-term (5-10 years of hormone use), there may be decreased risk for:
- Cardio-vascular disease
- All-cause mortality
- Osteoporosis & bone breaks from Osteoporosis
-Hormone therapy is best for prevention rather than treatment of Osteoporosis - Colon cancer
Side effects & risks
Short-term:
- Spotting & bleeding
- Breast tenderness
- Bloating
- Water retention
- Nausea
- Headaches
Longer-term risks vary depending on health history, age, dose and form of medication. There is a somewhat greater risk with higher doses and oral administration (versus transdermal).
- Blood clots & Stroke
-Risk for blood clot & stroke are formulation dependent, with oral estradiol showing a modest correlation, but many studies reporting that standard, low-dose transdermal & vaginal formulations may be safer options - Breast cancer incidence
-Those who use estrogen alone have a lower risk than the general population
Non-hormone interventions
There is not a large body of research on the benefits of other treatments outside of HT, and most studies explore hot flashes and night sweats. Currently, there are no supplements approved for the treatment of Menopause. Each person will require a unique combination of medical, holistic and lifestyle options for relief and maximum well-being. It is recommended that women keep track of:
- Symptoms
- Triggers
- What works to improve symptoms
There are some alternative treatments with reasonable data support that are recommended by the Menopause Society:
- Cognitive behavioral therapy (CBT)
- Hypnosis (especially for sleep disturbance)
There are other low risk interventions that have a less robust research foundation, but anecdotal, positive benefits:
Modifiable risk factors

We know that risk for certain diseases (cardiac, musculoskeletal, cognitive, cancer) increases with age, because of or in combination with menopause. It can only be beneficial to take steps to limit these conditions, regardless of your decision about utilizing HT.
- Maximize brain health
- Reduce stress
- Monitor & control cholesterol & blood pressure with lifestyle habits (diet and exercise) or medications as needed. These variables have direct effects on cardiac and stroke risk
- Improve your sleep
- Limit your intake of alcohol and processed or other unhealthy foods
- Limit bone loss & injury risk with:
– Adequate intake of calcium & vitamin D
– A healthy diet
– Infusion
– Weight training & balance exercises
Resources
- BWH – Menopause and Midlife Clinic
- MGH – Midlife Women’s Health Center
- Menopause Society – Menopause Map
- The Menopause Charity
- Red Hot Mamas Menopause Support Group
- The Flow Space Menopause Apps & Symptom Trackers
- Podcasts
Other Women’s Health Features
Help from the EAP
We offer free and confidential services for employees and immediate household family members. EAP records are separate from medical and HR records. Contact the EAP at 866-724-4327 or request an appointment via our online form for confidential assistance. In-person appointments are available at the following locations. Phone or Video (Zoom) appointments are available from all locations.
* The content in this news feature is intended for informational purposes and is not meant to provide any specific clinical guidance. Every health care situation is unique and best addressed in consultation with your provider.