Understanding Long COVID
Stacey J. Drubner, JD, LICSW, MPH

EAP Ask the Expert: David Systrom, MD, Director – Dyspnea Clinic & Advanced Cardiopulmonary Exercise Testing Program, Co-Director, Ronald G. Thompson Harvard ME/CFS Collaboration, Brigham & Women’s Hospital
What is Long COVID?
You may have heard about or know of someone who has Long COVID, also referred to as post-acute sequelae of SARS-CoV-2 (PASC). But 5 years after the Pandemic began, how much do we understand about Long COVID in terms of causes, diagnosis, or treatment? Getting clear answers is complicated due to:
- A continuum of diverse symptoms, severity & recovery paths
- The fact that it is a disease of clinical impression, with no universal biomarker
- Data collection barriers – less formal reporting & testing, comorbidities
- Evolving research
- A significant clinician learning curve, with limited treatment hubs
- Potential stigma, due to all the above
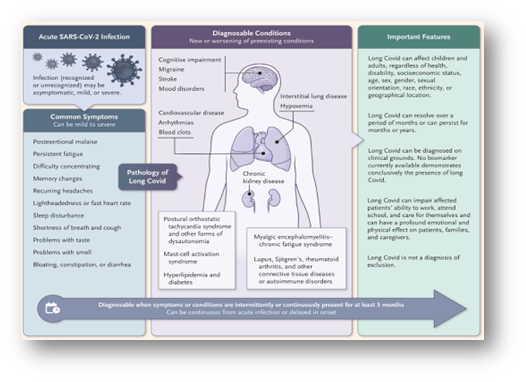
There is a working definition – Long Covid is an infection-associated chronic condition that occurs after SARS-CoV-2 infection and is present for at least 3 months as a continuous, relapsing and remitting, or progressive disease state that affects one or more organ systems. You can find more information here and in the diagram below.
We are fortunate to be able to tap into the specialized expertise of David Systrom, MD, pulmonologist, and researcher from BWH, to better understand the most current wisdom on Long COVID.* Dr. Systrom also has considerable experience with Chronic Fatigue Syndrome (ME/CFS), which has some similar disease pathways and clinical presentations.
How Common is Long COVID?
The statistics show a range, with significant variability:
- CDC – About 7% of US adults reported having Long COVID (2022)
- KFF – Shows rates falling with 3/10 reported ever having Long COVID, with 1/10 reporting they still have it (2024)
- MGB – Early phase AI research shows a potentially higher rate (22.8%) which may be due to under-reporting/diagnosing, related to access issues or bias (2024)
On the positive side, we may have entered a phase with less new cases of Long COVID. Dr. Systrom hypothesizes that more (but certainly not all) cases of Long COVID are attributable to initial infections and earlier, more virulent strains. One significant risk factor, having had a severe case of COVID, is less common in today’s cohort of patients.
Symptoms and Impacts of Long COVID
Regardless of the exact numbers, a substantial number of people are not only coping with impacts on physical and emotional health, but also with challenges related to employment, financial well-being, and relationships. Some of the most common symptoms (of which there are 200 and counting) or side effects are listed below.

- Brain fog, memory & cognition
- Cough or shortness of breath
- Fibrosis of the lungs
- Fatigue & low energy
- Fever
- Headaches
- Joint pain
- Heart or blood vessel damage
- Blood clots
- Low, or less commonly, high blood pressure
- Gastrointestinal problems
- Loss of smell/taste or other impacts on these senses
- Depression, anxiety, PTSD (primary or secondary)
- Sleep disturbance
- Appetite issues
- Lifestyle & activity limitations
Populations that are Most at Risk for Long COVID

Reported rates are the highest among the following groups:
- Older individuals
- Females
- Hispanic, Latinos & Whites
- Individuals with co-morbidities or high-risk medical conditions (heart or lung disease, diabetes, obesity, allergies, other auto-immune diseases)
- Those with disabilities
- Individuals who have had a severe case of COVID
Diagnosing or Identifying an Explanation for Long COVID

As mentioned above, there are different presentations of Long COVID and currently no definitive test or biomarker. Dr. Systrom hopes that future research will uncover a number of biomarkers for the distinctive pathways and physiologies, leading to a knowledge base for precision medicine for diagnosis and treatment.
In the meantime, Long COVID will continue to be diagnosed via clinical impression through a comprehensive evaluation, which includes determining how activities impact symptoms. A starting point is a positive COVID test, (preferably PCR but not required outside of the research space), combined with unexplained or persistent symptoms (referenced above). The current hypotheses for the most debilitating symptoms, such as respiratory issues, fatigue, and brain fog relate to unbridled inflammation and blood flow (vascular) issues. Below, we include a brief review of some research that supports these theories.
Continuing presence of the COVID virus in the system
Some (43%) individuals with Long COVID still show virus-derived proteins within 14 months of their initial diagnosis. In other words, the antigen (or marker) for COVID is still present. This could certainly lead to a prolonged state of inflammation, which is associated with both infection and uncomfortable side effects.
Blood flow issues which lead to oxygen deficits and symptoms induced by exercise
- Research at BWH with Dr. Systrom and colleagues using Invasive Cardio-pulmonary Exercise Testing, to measure breathing, ventilation and pulmonary functioning, has shed light on symptoms of exercise intolerance (fatigue, shortness of breath, and potentially brain fog). In patients with Long COVID, there was evidence of vascular issues, with low pressure filling the heart. Muscles needed for exercise did not get adequate oxygen. Instead, blood flow (and oxygen) was distributed to places that do not need this, such as the skin, kidneys, or gut.
- A study out of Amsterdam, involved doing a biopsy of muscle tissue of women with Long COVID, and concluded that mitochondria needed for energy are not functioning properly, leading to poor oxygen uptake during exercise. The practical result is that patients experience fatigue with exertion.
- A small study out of South Africa found high levels of inflammatory molecules “trapped” in micro-clots observed in Long COVID patients, which may be preventing the breakdown of clots. This may also contribute to issues with healthy oxygen processes which can cause fatigue and other pulmonary problems.
Can Long COVID be Prevented?
Diagnosis and treatment of illness should not involve blame or shame, but there may be things that can reduce chances of getting Long COVID. Dr. Systrom points out that key to this is to avoid getting acute COVID, a major risk factor for Long COVID.
- Follow the recommendations (handwashing & masking around sick people) to prevent contracting any respiratory diseases, in the first place.
- Keep high-risk co-morbidities (diabetes, obesity) in check via lifestyle habits or adhering to medical recommendations, such as being compliant with prescribed medications.
- Experts believe that vaccines can help prevent serious COVID, but there is no consensus about whether vaccines prevent Long COVID.
-One study with the veteran population reported that initial series vaccines prevented Long COVID with early strains of the disease.
-More recent research seems to indicate that vaccines do not coincide with preventing Long COVID.
-Dr. Systrom referenced a rare, small subset who has “Long Vax Syndrome” leading to Long COVID after vaccination. This may be attributable to an immune system overload response. - Some observational studies indicate that use of antivirals such as Paxlovid (which can prevent more serious illness) may reduce incidences of Long COVID. Clinical trials are recommended to study this more fully.
Recovering from COVID
 About one-third of individuals with some form of Long COVID recover without seeking medical care. There is little clarity on what percentage of people who receive treatment go into full remission. However, Dr. Systrom indicates that there are options that provide at least partial improvement and anecdotal reports show patients who appear to return to baseline with some of the interventions discussed below.
About one-third of individuals with some form of Long COVID recover without seeking medical care. There is little clarity on what percentage of people who receive treatment go into full remission. However, Dr. Systrom indicates that there are options that provide at least partial improvement and anecdotal reports show patients who appear to return to baseline with some of the interventions discussed below.
Medications & Supplements
Currently, there are no FDA approved medications for Long COVID, but there are some off- label uses of existing medications that are either in trial and/or being evaluated in Long COVID clinics.
A common goal with these interventions is to check unbridled inflammation and normalize blood flow in the vascular system. Improvements have been observed in symptoms such as fatigue, shortness of breath and lightheadedness.
- Individual or combination use of low dosage of Naltrexone (used to treat addiction in larger doses), and Mestinon/Pyridostigmine (used to treat an auto-immune disease, Myasthenia Gravis)
- Transdermal nicotine patches affect receptors which may help decrease inflammation, and improve autonomic functions like blood pressure, breathing, and cognition
- Mitochondrial vitamin cocktail (Riboflabin, CoQ10, Alpha light folic acid)
- Rampamycin which is anti-inflammatory
- Antihistamines (H1 and H2 blockers), which can be used to tamp down the overactivation of the immune system’s mast cells in tissues and address nerve damage
- Probiotics to counteract damage to the microbes of the gut
Coaching around exercise & exertion
Dr. Systrom stresses that extreme caution should be used in managing exertion with graded exercise programs (gradually increasing exertion). Mainstream medicine has a tendency to assume that fatigue related to Long COVID or Chronic Fatigue Syndrome is a function of being out of shape. While it’s true that Deconditioning will not help any chronic disease, simply sending people to the gym isn’t going to fix Long COVID. This strategy results in greater fatigue and brain fog (post-exertional malaise). Dr. Systrom recommends addressing this with a combination of medication and a conservative, gradual graded exercise program. This will help to avoid post-exertion malaise and will increase functionality overall.

Holistic & other lifestyle interventions
Dr. Systrom favors having data from robust clinical trials before endorsing any intervention as having definitive benefits. Despite that caveat, he does not automatically invalidate patient accounts of examples of things that were effective for them. This might include a gluten-free diet, acupuncture, or mind-body activities. We have discussed the impact of the mind-body connection in other EAP features.
Getting Help for Long COVID
Patients, families, and providers should not shy away from seeking or offering help just because current information about Long COVID is new and evolving. Research has shown that it is not an imaginary condition. There are options for relief which can be better studied and fine-tuned with increased identification of those in the Long COVID population.
Dr. Systrom cautions that we need to be mindful of potential disparities in diagnosis or treatment for those who are disenfranchised in the medical system, via barriers related to access, coverage, cultural norms, or bias.
The best ways to address disparities is through clinician education, patient outreach, and public health messaging. Validation will help to encourage people to speak up and seek assistance.
If you have had COVID and have symptoms that seem persistent, unexplained, and concerning, do not hesitate to reach out for help, either from your PCP or one of the specialty centers listed below.

Long COVID centers
- BIDMC – Critical Illness and COVID-19 Survivorship Program
- BMC – ReCOVer Long COVID Clinic
- BWH – COVID Recovery Center
- Emerson Health – COVID-19 Recovery Program
- SRH Salem – COVID Rehabilitation Program
Peer-led Support
- Facebook – Long COVID Support Group
- Facebook – Long Covid & Pregnancy
- Mayo Clinic – Post-COVID Recovery & COVID-19 Support Group
Guidance for Providers
Other Long COVID Resources
Help from the EAP
If you or a colleague are struggling with the emotional impacts of coping with Long COVID or any medical illness, the EAP is here to help. We offer free and confidential services for employees and immediate household family members. EAP records are separate from medical and HR records. Contact the EAP at 866-724-4327 or request an appointment via our online form for confidential assistance. In-person appointments are available at the following locations. Phone or Video (Zoom) appointments are available from all locations.
* The content in this news feature is intended for informational purposes and is not meant to provide any specific clinical guidance. Every health care situation is unique and best addressed in consultation with your provider.